New Project Launches to Expand AI-Powered Cancer Care Operations Across Canada
Dec 16, 2025
Building on the success of a previous collaboration, an expanded pan-Canadian consortium of health institutions has launched a new initiative to bring advanced prediction and operational decision-support capabilities to cancer centres nationwide.
The initiative was formally announced on December 16, 2025, at a Scale AI ecosystem event in Toronto.
Cancer centres are under unprecedented pressure: rising patient volumes, frequent last-minute changes, and limited tools to manage operational complexity all contribute to avoidable delays and unused capacity. In radiation therapy, previous analyses have shown that centres often operate below their true capacity, with nearly 30% of potential throughput left unused due to operational constraints.
Following the proven impact of a previous project funded by Scale AI, which demonstrated efficiency gains equivalent to treating nearly 1,000 additional patients per year and delivered significant cost savings, a new national initiative officially launched in August 2025.
This new phase brings together The Ottawa Hospital, the McGill University Health Centre, CancerCare Manitoba, Gray Oncology Solutions, and partner institutions including the Princess Margaret Cancer Centre, the CHUM, the CISSS de Laval, the CIUSSS de l’Est-de-l’Île-de-Montréal, the Jewish General Hospital, the Southlake Regional Health Centre, and the CIUSSS de l’Estrie – Sherbrooke. Supported by Scale AI, the consortium is focused on strengthening the operational resilience of cancer care across Canada.
What’s New in 2025?
The 2025 project expands both the scope and the ambition of the original initiative. It will:
Refine predictive models developed in 2023 (patient flow, cancellations, appointment durations).
Transform these predictions into operational recommendations that managers can directly act on.
Introduce new capabilities such as automated rescheduling and crisis management to better handle disruptions.
Scale adoption across more hospitals, extending GrayOS’s impact nationally.
Together, these advancements move GrayOS from predicting operational issues to prescribing actionable adjustments to resolve them; the defining capability of a true Care Orchestration Platform.
From Prediction to Prescription: The New AI Engines Powering GrayOS in Radiation Therapy and Systemic Therapy
This project introduces three major capabilities that give radiation and systemic therapy teams the visibility, control, and resilience needed to run complex cancer programs more efficiently:
Control Tower
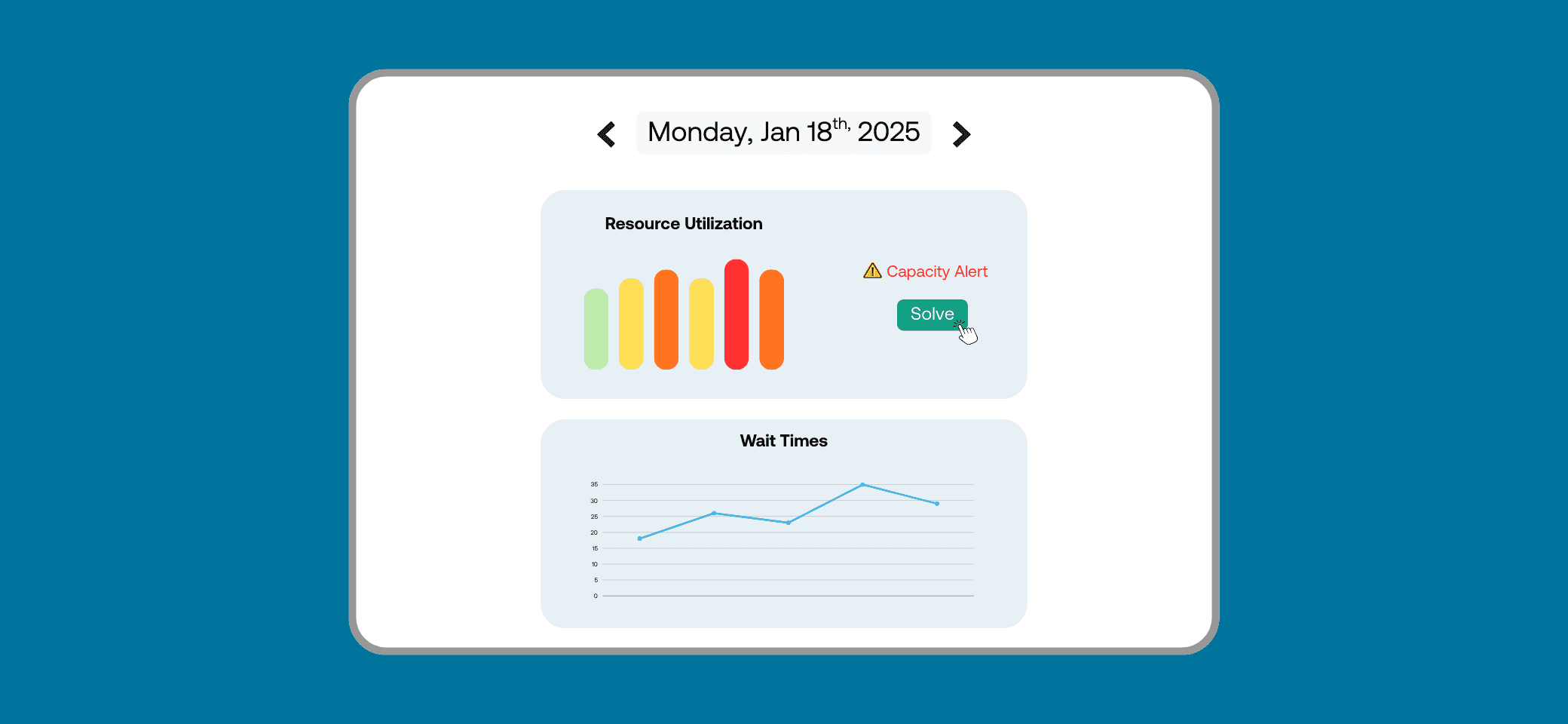
The Control Tower View will become the central workspace for operational leaders. It provides a live, color-coded capacity timeline of every critical resource (showing at a glance where bottlenecks will occur and where unused capacity exists). Managers will be able to test operational policies, such as adjusting operating hours or compressing appointment durations toward predicted values, and see in real time how those changes affect patient delays, overtime, and utilization. This turns long-range planning into an interactive, data-driven process, giving leaders control over both the benefits and risks of their decisions.
Crisis Management Tool
Even the best plan faces unexpected disruptions (a machine breakdown, sudden staff absence, or urgent patients arriving without notice). The Crisis Management Tool will provide a guided workflow to handle these emergencies with confidence. Users will be able to declare a crisis, identify affected appointments, and receive step-by-step recommendations on which patients can be safely delayed, reassigned, or clustered. By temporarily unlocking extra efficiency or extending operating hours, the system helps leaders resolve disruptions quickly without sacrificing patient care or operational stability.
Intelligent Rescheduling
In systemic therapy, higher-priority patients often need timely treatment, yet full schedules and sudden nurse absences make rescheduling a manual, stressful task. The new Rescheduling Engine will automate this process. It will weigh patient priorities, dependencies (labs, consults), drug clustering, and individual constraints to generate optimized rescheduling proposals. In practice, this means urgent patients can start sooner, staff can respond more effectively to last-minute absences, and departments can reduce the domino effect of reactive cancellations.
“Thanks to this innovative project, nurses who previously spent time scheduling will be able to dedicate more time to being at the bedside where they are most needed. This is a great example of how artificial intelligence can help us improve efficiency while maintaining the highest standards of care.”
Dr. Lucie Opatrny, President and Executive Director, MUHC
“Improving access to cancer treatment requires more than new equipment; it requires smarter, more adaptive systems. This initiative will help care teams respond to disruptions in real time, reduce wasted capacity, and ensure that more patients receive timely, uninterrupted treatment. The GrayOS Control Tower represents a meaningful step toward a more resilient, efficient, and patient-centred oncology system across Canada.”
Suzanne Comino, supervisor, Radiation Therapy Program, TOH
“This project marks a turning point for oncology operations. For years, cancer centres have lacked the tools to manage complexity with precision. By moving from operational prediction to operational prescription, we are giving care teams the ability to act proactively instead of reactively. The goal is simple: ensure that no patient waits unnecessarily because of operational constraints. This project accelerates our vision of a true Care Orchestration Platform: one that strengthens resilience, supports clinical teams, and expands access to timely, high-quality cancer care across the country.”
André Diamant, CEO, Gray Oncology Solutions
Why It Matters
For operational leaders, this means gaining real-time, data-driven decision support to optimize resources, prioritize urgent patients, and strengthen resilience during crises. By embedding AI into the logistics of cancer care, the project aims to ensure that health systems can do more with the same resources, supporting both patients and staff.